MIPS & QPP Highlights & Flexible Options for Care Providers
This post is part of a MACRA Monday series where we dive into the details of the MACRA Quality Payment Program.
The Centers for Medicare and Medicaid Services (CMS) recently released a Proposed Rule highlighting recommended updates to the 2018 reporting period of the Quality Payment Program (QPP). Like flexibilities extended in 2017, the proposal seeks to further reduce reporting burdens on small practices and rural providers in the program’s second-year reporting period.
Merit-based Incentive Payment System (MIPS) reporting track updates include:
- Increased low-volume exemption thresholds (<200 patients or <$90,000 in payments)
- New virtual group options for solo practitioners and groups with 10 or fewer Eligible Clinicians
- Extending “pick your pace” flexibilities into 2018\
- Postponing introduction of the Cost category to MIPS composite scores
- Factoring MIPS performance improvements into quality scores
- Permissions for facility-based providers to report through the facility where they do most of their work instead of the practice
- Permitting the use of 2014 CEHRT in 2018 reporting
The Rule introduces new MIPS bonus point opportunities for:
- The use of 2015 CEHRT
- The care of complex patients
Recommendations also extend small practice relief including:
- Up to 5 bonus points for practices with 15 or fewer Eligible Clinicians
- Hardship exemption for Advancing Care Information category measures
- Additional points on Quality measures that don’t meet completeness requirements
Comments on the Proposed Rule are due by August 21, 2017. Physicians have until October 2, 2017, to begin collecting performance data for the inaugural 2017 MIPS reporting period.
Calculating MIPS: The Financial Impact on Specialty Practices
Results from a crowdsourced survey fielded by Black Book Research among nearly 9,000 physician practices from February through April of 2017 reveal that 94 percent of physician participants were unaware or unsure of how to predict their 2017 MIPS performance scores. Seventy-seven percent of practices with three or more clinicians reported intentions to purchase MIPS compliance technology solutions by the fourth quarter of this year, largely driven by an inability to independently determine earning potential under MACRA.
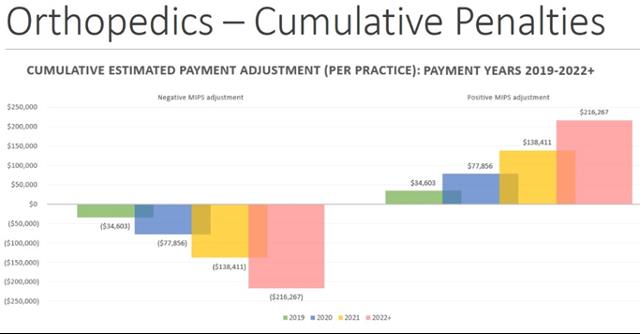
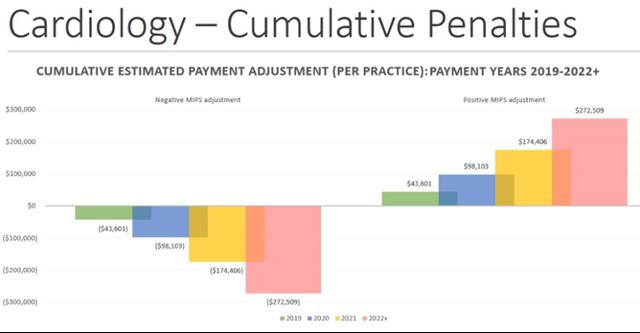
Orthopedics, cardiology and radiology are among the highest incentivized specialties under MIPS. To help specialty practices quantify the fiscal impact MIPS poses, we evaluated average Medicare earnings by specialty to establish the MIPS calculations below. These estimates are based on bare minimum earnings and losses that could be greater for practices with larger Medicare patient populations and/or more physicians. (Calculations are strictly illustrative estimates.)
Cardiology Practices
Estimated average payment adjustment for a 5-clinician cardiology practice in 2019 alone: $43,601
Number of cardiology-specific QPP measures: 20
Orthopedics Practices
Estimated average payment adjustment for a 6-clinician orthopedics practice in 2019 alone: $34,603
Number of orthopedics-specific QPP measures: 21
Radiology Practices
Estimated average payment adjustment for a 6-clinician radiology practice in 2019 alone: $30,117
Number of radiology-specific QPP measures: 22
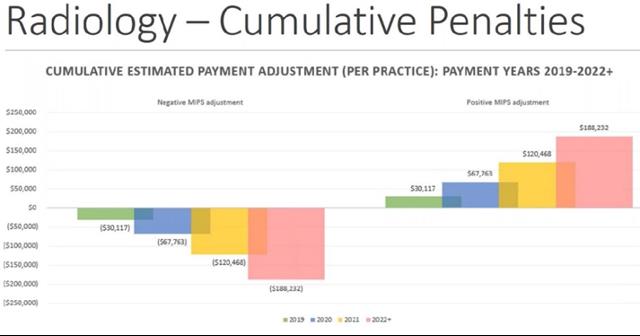
Note: The above projections assume the full incentive and penalty will be paid out as outlined in the MACRA law. However, the positive and negative payment adjustments will be scaled so the program is budget neutral. This means that the positive payment adjustments will have to be offset by penalties.
Navigating the Transition to MIPS
As clinicians prepare for reporting under MIPS, establishing specialty-specific expertise on financial, clinical and technical objectives can help practices thrive rather than just survive.
Tips as you for prepare for MIPS:
- Know your reporting options and pick your path.
- Choose measures that play to the strengths of your specific specialty practice. Review your current billing codes and Quality and Resource Use Report to help determine these areas.
- Do a technology asset inventory to make sure you can track the required CQMs.
- Customize your EHR for track your selected measures or ID an outsource vendor to assist.
- Work towards minimum reporting requirements to avoid a penalty with a stretch goal to report on the full required measures to maximize positive adjustment earnings potential.
Additional resources:
QPP website: An overview and support documentation is available at the CMS QPP website here.
MIPS EDU Program: A new “Quality Payment Program in 2017: Pick Your Pace Web-Based Training” course with Continuing Education Credit is available through the Learning Management System. Learn more here.
2017 CMS-Approved Qualified Clinical Data Registries: Additional specialty-specific measures are available via approved 2017 QCDRs to meet MIPS reporting requirements. Options for cardiology, radiology and orthopedic practices are included. Learn more here.